BACKGROUND
Non-Hodgkin Lymphomas (NHL) represent one of the most common cancers in the United States, accounting for about 4% of all cancers and it is estimated over 77,000 people (including children and adults) will be diagnosed with NHL in the United States in 2020. Depending on the data, it is estimated T-cell lymphomas make up anywhere from 7 to 15% of all NHLs. Given their relative rarity compared to other sub-types of lymphomas (and malignancies at large), there is a scarce literature regarding their outcomes in ethnic minority groups. Retrospective reviews of cancer registries and SEER databases have demonstrated conflicting evidence regarding outcomes in Hispanics (HI) with some studies suggesting worse overall survival (OS) in this group (Clin Lymphoma Myeloma Leuk. PMID: 26198444), while others suggest comparable outcomes in the setting of healthcare homogeneity (Leuk Lymphoma. PMID: 25012944).
MATERIALS/METHODS
This is a retrospective study of a cohort of patients diagnosed with T-cell NHL from the Texas Cancer Registry (2006-2016). Patients were identified by the International Classification of Diseases for Oncology Third Edition (ICD-O-3) code list. Data was provided to us completely de-identified. Key variables collected included gender, ethnicity, dates at diagnosis and death, payer, stage, treatment, and poverty index. Categorical outcomes were summarized with frequencies and percentages and age, the only continuously distributed outcome, with the mean and standard deviation. The significance of variation in distribution of categorical outcomes with ethnicity [HI, non-Hispanic (NH)] was assessed with Fisher's Exact tests or Pearson's Chi-square as appropriate; age was assessed with T-test or Wilcoxon. Survival time was measured in years from date of primary diagnosis to date of death. Survival distributions were described with Kaplan-Meier curves and significance of variation in median survival with ethnicity was assessed with log rank testing. At risk tables were computed based on the Kaplan-Meier estimate of the survival curve. All statistical testing was two-sided with a significance level of 5%. Corrections for multiple testing were not applied. The R language was used throughout.
RESULTS
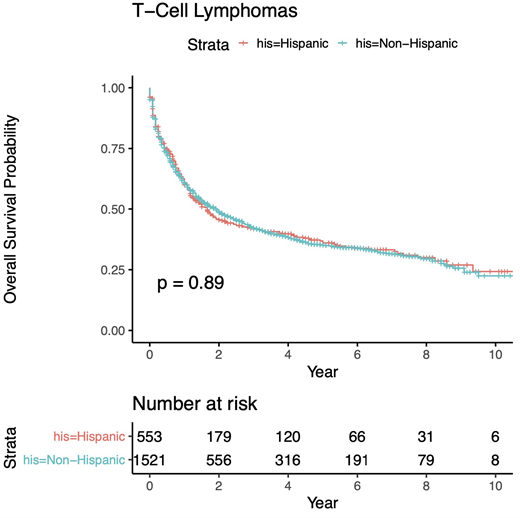
We identified 2074 patients with T-cell NHL (n= 902 Peripheral T Cell, NOS; 295 Angioimmunoblastic T Cell; 577 Anaplastic Large T Cell; 120 NK/T-cell; and 180 Adult T-cell Leukemia/Lymphoma). 553 were HI (26%), 1521 NH (74%). Median age of diagnosis in HI was 50.1 vs 57.4 in NH (p = <0.001). Males were more frequently affected, 63.8% in HI vs 58.9% in NH (p = 0.048). Most frequent poverty index was 20-100% for HI vs 10-19.9% for NH (p < 0.001). Most frequent payor for both groups were Medicare with 24.3% in HI vs 35.3% in NH (p < 0.001). Most common stage at diagnosis in both groups was III/IV with 50.3% in HI vs 49.7% in NH (p = 0.031). Most frequent chemotherapy included multiple agents for both, 55.7% in HI vs 44.2% in NH (p < 0.001). Majority in both groups had neither hematologic transplant 90.2% in HI vs 85.3% in NH (p = 0.073) nor radiation, 84.4% in HI vs 82.9% in NH (p = 0.076). Median overall survival (OS) in HI was 1.7 years vs 1.9 in NH; survival probability for HI vs NH at 2 years was 0.46 vs 0.49, at 5 years 0.37 vs 0.35, and at 10 years 0.24 vs 0.23 with no statistically significant difference in OS probability (p=0.89).
CONCLUSION
Our study demonstrates that amongst the population of Texas, HI with T-cell NHL have similar outcomes when compared to their NH counterparts. Breakdown of our cohort demonstrated similar healthcare utilization, as well as diagnostic and treatment modalities amongst both groups. Within the context of healthcare equality, we ascertained similar outcomes amongst groups, which is in agreement with previous reports claiming homogeneity of medical care helps overcome ethnic disparities.
Diaz Duque:ADCT Therapeutics: Research Funding; Molecular Templates: Research Funding; AstraZeneca: Research Funding; Hutchinson Pharmaceuticals: Research Funding; Seattle Genetics: Speakers Bureau; Verastem: Speakers Bureau; AbbVie: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.